#Heart Failure Market
Explore tagged Tumblr posts
Text
Top Trends in the Heart Failure Major Market for 2024
Heart failure (HF) remains a significant global health concern, affecting millions and imposing a heavy burden on healthcare systems. However, the landscape of the heart failure market is undergoing a dynamic transformation, driven by innovation and a growing focus on improved patient outcomes.
Buy Full Report to Know More About the Heart Failure Market Forecast
Download a Free Report Sample
Here's a glimpse into the top trends shaping this market in 2024:
1. The Rise of Minimally Invasive Interventions:
Minimally Invasive Valve Replacement (MIVR): Traditional open-heart surgery for valve replacement is being challenged by MIVR procedures. These minimally invasive techniques offer faster recovery times, reduced patient discomfort, and potentially improved long-term outcomes.
Transcatheter Aortic Valve Replacement (TAVR): TAVR is a well-established MIVR option for aortic valve stenosis, particularly for high-risk patients who may not be suitable for open-heart surgery. Advancements in technology are enabling broader patient application of TAVR procedures.
Percutaneous Mitral Valve Repair (PMVR): PMVR is a newer technique gaining traction for mitral valve regurgitation. This minimally invasive approach offers a less invasive alternative to traditional mitral valve surgery.
2. Precision Medicine and Personalized Care:
Genetic Testing and Tailored Therapies: Identifying the underlying genetic causes of heart failure allows for more targeted treatment approaches. This could involve personalized medication regimens or therapies aimed at addressing specific genetic risk factors.
Remote Monitoring and Telehealth Solutions: Wearable devices and remote monitoring technologies allow for continuous patient monitoring, enabling early detection of potential complications and facilitating timely interventions. Telehealth consultations offer improved access to specialist care, particularly in remote areas.
3. The Growing Focus on Heart Failure Prevention:
Early Detection and Risk Management: Emphasis is shifting towards early detection of heart failure risk factors like hypertension, diabetes, and obesity. This allows for lifestyle modifications, medication management, and preventative measures to potentially delay or even prevent the onset of heart failure.
4. Innovation in Cardiac Devices and Technologies:
Next-Generation Ventricular Assist Devices (VADs): VADs are implanted pumps that assist the heart in pumping blood. Advancements in VAD technology are leading to smaller, more efficient, and quieter devices with improved long-term outcomes for patients.
Artificial Intelligence (AI) in Diagnostics and Treatment: AI algorithms are being used to analyze patient data, predict potential complications, and personalize treatment plans. AI-powered tools can also assist with early detection of heart failure based on medical scans or patient monitoring data.
5. Evolving Healthcare Delivery Models:
Focus on Value-Based Care: There's a growing emphasis on healthcare models that focus on patient outcomes and value delivered, rather than simply volume of procedures. This incentivizes the development of more effective and cost-efficient treatment strategies for heart failure.
The Rise of Cardiac Rehabilitation Programs: Comprehensive cardiac rehabilitation programs play a crucial role in improving patient outcomes and quality of life after a heart failure event. These programs combine exercise therapy, education, and psychological support to help patients manage their condition and live longer, healthier lives.
Conclusion:
The heart failure market is brimming with promising advancements. The focus on minimally invasive procedures, personalized care, preventative measures, and innovative technologies offers hope for improved patient outcomes and a brighter future for those living with heart failure. As these trends continue to evolve, the heart failure market will play a vital role in alleviating the burden of this global health challenge.
1 note
·
View note
Text
I wish I could pull off crunchy art but I just don't think I can. I could try I guess that's what the spirit of Dogcember is all about. Practice. Exploration. Etc.
#its also a matter of what would people like to see? is there a market for this? etc#i really really like drawing dogs is the thing#im planning a very tiny test print of stickers coming up#and i havent decided on breeds yet... its just to test the waters but i feel id be setting myself up for failure#if i did /exclusively/ rare breeds lmao#which are the breeds i like to draw and represent in my work#the joy in my heart reading thru the comments on the announcement page for the npdd poster#all the people excited that someone /finally/ drew a nob#makes me so so happy#like thats the point!! thats why i draw rare breeds!#that and because i love love love to educate people who are less familiar with them/the dog world#like yeah sure lets talk about CAOs! lets talk about beauces! lets talk about xyz breed!#i have a lot of very strong feelings about rare breeds and preservation breeding as you can gather#this turned into a tangent LOL#anyway if you read this far feel free to send me your thoughts!
2 notes
·
View notes
Text
Congestive Heart Failure Drugs Market Revenue Expected to Strengthen, Reaching USD 26.1 Billion by 2032 with a 14.3% CAGR from 2023 to 2032
Acumen Research and Consulting has recently published a research report on the Congestive Heart Failure Drugs Market for the forecast period of 2023 – 2032, wherein, the global market has been analyzed and assessed in an extremely comprehensive manner. The research report on the Congestive Heart Failure Drugs Market offers an extensive analysis of how the postoperative pain therapeutics landscape…
#Congestive Heart Failure Drugs Market#Congestive Heart Failure Drugs Market Growth#Congestive Heart Failure Drugs Market Share#Congestive Heart Failure Drugs Market Size#Congestive Heart Failure Drugs Market Trends
0 notes
Text
Interest Check. An Address to the Ommfs 🦅✨🦝
eh hmm *taps mic* 👉🎙️ My fellow Followers. my mutuals, the lovers of weird, fandom enjoyers, shitpost extraordinaries, curious folk alike, a nation of Ommfs.. ✨

I Bruter am Weird this blog *taps the sign* is Weird And Cool AF (not to Brag💅✨) and as per the ONLY lore bit disclosure: I'm a "functional" introvert, resident hijinks and shenanigans shitposter, a southern Bastard, creature connoisseur.. 😌 But. I am also now an individual with a chronic disease ..
I am diagnosed with Heart Failure ❤️🩹

Yeeaaah... 👉👈🙃

This blog has really never been about Me as an individual (I'm an introvert my self lore lockdown rivals national security lol), but I cant deny this dank hellsite for my rambles and hyper fixations has helped me be comfortable to be Me, the Real ME. An acespec, intersex, poc who likes monsters and gore maybe a tad too much.. just a Little🤏😅
The Point of this post is to not feel saddened or pity for me (I wont fault anyone that may express this). I have accepted the reality that I may not live a long life, but I refuse to live in Submission to my illness. I've made up my mind that if I must go then I'll Die On My Feet.
I'm humbly asking if there's Interest Check to follow along with me to achieve my Ideal Body. Another lore bit about me is I've always had a fairly active life and outdoorsman quality though amateurish. I want to take my body transformation more Seriously now. Work and learn to build my body to the form it Wants to be and I'd like to share this journey with yall, scratch out a roadmap, have fun trekking the yonder and hopeful.. No, Definitely achieve my goal maybe even More.

*deep inhale and exhale* 😤 OK. that was ALOT to get off my chest.. 💦 But do know that I'm OK. I have doctors, I have medicine and I'm as Stubborn as a Bulldog 🐾 Although I'm not rich by any means and NOW will live in a republican ran administration (*head in hands* lawdhamercy 🥲) I'm OK as ok can be���✨
#brutermonger speaks#heart disease#heart failure#long post#long ass post#dont mind me#personal#i got a bit emotional#it wont happen again#probably#back to being dead inside👍#sadman swagger✨#I will make a separate blog for body building#self improvement#I'll share health food and Fashion✨#drip marketing#incoming#health and wellness#healthylifestyle#bodybuilding#💪✨#friendly reminder capitalism wants us Dead#how will the republications shit on the terminally ill and disabled this time around???#🦝#local introvert overshares#doomed by the narrative#rambles#but we Move#followers
1 note
·
View note
Text
https://bundas24.com/read-blog/137837_congestive-heart-failure-drugs-market-size-overview-share-and-forecast-2031.html
The Congestive Heart Failure Drugs Market in 2023 is US$ 7.21 billion, and is expected to reach US$ 12.98 billion by 2031 at a CAGR of 7.60%.
#Congestive Heart Failure Drugs Market#Congestive Heart Failure Drugs Market Growth#Congestive Heart Failure Drugs Market Trends
0 notes
Link
0 notes
Text
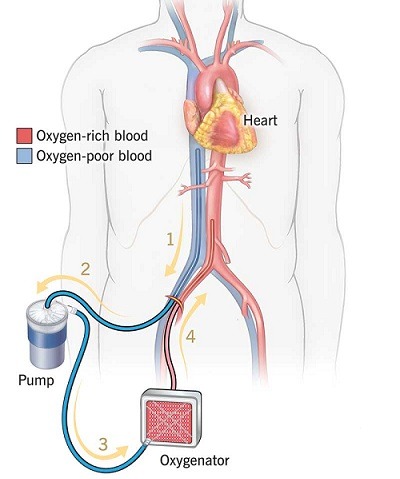
Extracorporeal Membrane Oxygenation Machine | Exploring Opportunities and Challenges
The global extracorporeal membrane oxygenation machine market size is anticipated to reach to reach USD 445.7 million by 2030, expanding at a CAGR of 5.5% from 2024 to 2030, based on a new report by Grand View Research, Inc. This growth can be attributed to the rising prevalence of cardiopulmonary and respiratory diseases, increasing adoption of ECMO machines in hospitals, and technological advancements in ECMO machines. The market expansion is also driven by the need for advanced life support technologies like ECMO machines, which are becoming increasingly necessary in treating patients with severe or life-threatening cardiac or pulmonary conditions.
Extracorporeal Membrane Oxygenation Machine Market Report Highlights
In 2023, the oxygenators segment accounted for the largest market share. This can be attributed due to prevalence of diseases like coronary heart disease and chronic obstructive pulmonary disease (COPD) continues to rise, the demand for advanced life support technologies like ECMO machines increases, driving the growth of the oxygenators segment.
The veno-arterial segment dominated the modality segment of ECMO machine market in 2023. This growth can be attributed due to high usage of veno-arterial ECMO in treating patients with cardiac arrest, where it assists with algorithm life support strategies to restore blood circulation. Additionally, the increasing incidence of chronic obstructive pulmonary disease (COPD) is also a key driver of this market segment.
The respiratory segment dominated the application segment in 2023 due to the high prevalence of respiratory diseases, such as Chronic Obstructive Pulmonary Disease (COPD) and acute respiratory distress syndrome (ARDS), which are leading causes of death worldwide, necessitate advanced life support technologies like ECMO machines.
The adult patient segment dominated the patient type segment in 2023 due to the prevalent incidence of heart and lung-related issues necessitating life-saving interventions.
The North American region held the largest share of the market in 2023 due to key industry players, consistent product launches, government backing for quality healthcare, advanced healthcare infrastructure, and favorable reimbursement policies.
Market players adopt several strategic initiatives to increase the product reach and improve availability in diverse geographic areas.
For More Details or Sample Copy please visit link @: Extracorporeal Membrane Oxygenation Machine Market Report
The rising prevalence of cardiovascular and respiratory diseases. Diseases such as coronary heart disease, cerebrovascular disease, rheumatic and congenital heart diseases, respiratory diseases like acute respiratory distress syndrome (ARDS), and chronic obstructive pulmonary diseases are leading causes of death worldwide. For instance, according to the World Heart Federation, approximately 18.6 million people die annually from cardiovascular diseases. Additionally, about 190,000 Americans are diagnosed with ARDS annually in the U.S. Such an increasing prevalence of cardiovascular and respiratory diseases has boosted the demand for ECMO machines, driving the market growth.
In addition, the increasing rate of technical improvement is increasing the usage of products. It is easier to transfer critically ill patients now as machine parts like hollow pumps and oxygenators are smaller. Moreover, introducing technologically advanced components, such as improved rotary pumps, dual-lumen cannulas, innovative oxygenators, and new cannulation approaches, is anticipated to ease the use of ECMO machines. For instance, in 2022, Inspira Technologies OXY B.H.N. Ltd. recently introduced the "Liby" System, an advanced life support system used to treat patients with life-threatening heart and lung failure. Similar advancements and the introduction of new products are expected to drive market growth in the coming years.
#extracorporeal membrane oxygenation#ECMO#life support technology#critical care#cardiopulmonary support#medical devices#intensive care#respiratory failure#heart-lung bypass#market analysis#healthcare technology#patient care#emergency medicine#global health#cardiac surgery#pulmonology#resuscitation#innovation#market trends#healthcare industry
0 notes
Text
Heart Failure Diagnostic And Monitoring Device Market Size Analysis 2023
0 notes
Text
#Heart Failure Poc & Loc Devices Market#Heart Failure Poc & Loc Devices Market Trends#Heart Failure Poc & Loc Devices Market Growth#Heart Failure Poc & Loc Devices Market Industry#Heart Failure Poc & Loc Devices Market Research#Heart Failure Poc & Loc Devices Market Report
0 notes
Text
Epic Systems, a lethal health record monopolist

Epic Systems makes the dominant electronic health record (EHR) system in America; if you're a doctor, chances are you are required to use it, and for every hour a doctor spends with a patient, they have to spend two hours doing clinically useless bureaucratic data-entry on an Epic EHR.
How could a product so manifestly unfit for purpose be the absolute market leader? Simple: as Robert Kuttner describes in an excellent feature in The American Prospect, Epic may be a clinical disaster, but it's a profit-generating miracle:
https://prospect.org/health/2024-10-01-epic-dystopia/
At the core of Epic's value proposition is "upcoding," a form of billing fraud that is beloved of hospital administrators, including the "nonprofit" hospitals that generate vast fortunes that are somehow not characterized as profits. Here's a particularly egregious form of upcoding: back in 2020, the Poudre Valley Hospital in Ft Collins, CO locked all its doors except the ER entrance. Every patient entering the hospital, including those receiving absolutely routine care, was therefore processed as an "emergency."
In April 2020, Caitlin Wells Salerno – a pregnant biologist – drove to Poudre Valley with normal labor pains. She walked herself up to obstetrics, declining the offer of a wheelchair, stopping only to snap a cheeky selfie. Nevertheless, the hospital recorded her normal, uncomplicated birth as a Level 5 emergency – comparable to a major heart-attack – and whacked her with a $2755 bill for emergency care:
https://pluralistic.net/2021/10/27/crossing-a-line/#zero-fucks-given
Upcoding has its origins in the Reagan revolution, when the market-worshipping cultists he'd put in charge of health care created the "Prospective Payment System," which paid a lump sum for care. The idea was to incentivize hospitals to provide efficient care, since they could keep the difference between whatever they spent getting you better and the set PPS amount that Medicare would reimburse them. Hospitals responded by inventing upcoding: a patient with controlled, long-term coronary disease who showed up with a broken leg would get coded for the coronary condition and the cast, and the hospital would pocket both lump sums:
https://pluralistic.net/2024/06/13/a-punch-in-the-guts/#hayek-pilled
The reason hospital administrators love Epic, and pay gigantic sums for systemwide software licenses, is directly connected to the two hours that doctors spent filling in Epic forms for every hour they spend treating patients. Epic collects all that extra information in order to identify potential sources of plausible upcodes, which allows hospitals to bill patients, insurers, and Medicare through the nose for routine care. Epic can automatically recode "diabetes with no complications" from a Hierarchical Condition Category code 19 (worth $894.40) as "diabetes with kidney failure," code 18 and 136, which gooses the reimbursement to $1273.60.
Epic snitches on doctors to their bosses, giving them a dashboard to track doctors' compliance with upcoding suggestions. One of Kuttner's doctor sources says her supervisor contacts her with questions like, "That appointment was a 2. Don’t you think it might be a 3?"
Robert Kuttner is the perfect journalist to unravel the Epic scam. As a journalist who wrote for The New England Journal of Medicine, he's got an insider's knowledge of the health industry, and plenty of sources among health professionals. As he tells it, Epic is a cultlike, insular company that employs 12.500 people in its hometown of Verona, WI.
The EHR industry's origins start with a GW Bush-era law called the HITECH Act, which was later folded into Obama's Recovery Act in 2009. Obama provided $27b to hospitals that installed EHR systems. These systems had to more than track patient outcomes – they also provided the data for pay-for-performance incentives. EHRs were already trying to do something very complicated – track health outcomes – but now they were also meant to underpin a cockamamie "incentives" program that was supposed to provide a carrot to the health industry so it would stop killing people and ripping off Medicare. EHRs devolved into obscenely complex spaghetti systems that doctors and nurses loathed on sight.
But there was one group that loved EHRs: hospital administrators and the private companies offering Medicare Advantage plans (which also benefited from upcoding patients in order to soak Uncle Sucker):
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8649706/
The spread of EHRs neatly tracks with a spike in upcharging: "from 2014 through 2019, the number of hospital stays billed at the highest severity level increased almost 20 percent…the number of stays billed at each of the other severity levels decreased":
https://oig.hhs.gov/oei/reports/OEI-02-18-00380.pdf
The purpose of a system is what it does. Epic's industry-dominating EHR is great at price-gouging, but it sucks as a clinical tool – it takes 18 keystrokes just to enter a prescription:
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2729481
Doctors need to see patients, but their bosses demand that they satisfy Epic's endless red tape. Doctors now routinely stay late after work and show up hours early, just to do paperwork. It's not enough. According to another one of Kuttner's sources, doctors routinely copy-and-paste earlier entries into the current one, a practice that generates rampant errors. Some just make up random numbers to fulfill Epic's nonsensical requirements: the same source told Kuttner that when prompted to enter a pain score for his TB patients, he just enters "zero."
Don't worry, Epic has a solution: AI. They've rolled out an "ambient listening" tool that attempts to transcribe everything the doctor and patient say during an exam and then bash it into a visit report. Not only is this prone to the customary mistakes that make AI unsuited to high-stakes, error-sensitive applications, it also represents a profound misunderstanding of the purpose of clinical notes.
The very exercise of organizing your thoughts and reflections about an event – such as a medical exam – into a coherent report makes you apply rigor and perspective to events that otherwise arrive as a series of fleeting impressions and reactions. That's why blogging is such an effective practice:
https://pluralistic.net/2021/05/09/the-memex-method/
The answer to doctors not having time to reflect and organize good notes is to give them more time – not more AI. As another doctor told Kuttner: "Ambient listening is a solution to a self-created problem of requiring too much data entry by clinicians."
EHRs are one of those especially hellish public-private partnerships. Health care doctrine from Reagan to Obama insisted that the system just needed to be exposed to market forces and incentives. EHRs are designed to allow hospitals to win as many of these incentives as possible. Epic's clinical care modules do this by bombarding doctors with low-quality diagnostic suggestions with "little to do with a patient’s actual condition and risks," leading to "alert fatigue," so doctors miss the important alerts in the storm of nonsense elbow-jostling:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5058605/
Clinicians who actually want to improve the quality of care in their facilities end up recording data manually and keying it into spreadsheets, because they can't get Epic to give them the data they need. Meanwhile, an army of high-priced consultants stand ready to give clinicians advise on getting Epic to do what they need, but can't seem to deliver.
Ironically, one of the benefits that Epic touts is its interoperability: hospitals that buy Epic systems can interconnect those with other Epic systems, and there's a large ecosystem of aftermarket add-ons that work with Epic. But Epic is a product, not a protocol, so its much-touted interop exists entirely on its terms, and at its sufferance. If Epic chooses, a doctor using its products can send files to a doctor using a rival product. But Epic can also veto that activity – and its veto extends to deciding whether a hospital can export their patient records to a competing service and get off Epic altogether.
One major selling point for Epic is its capacity to export "anonymized" data for medical research. Very large patient data-sets like Epic's are reasonably believed to contain many potential medical insights, so medical researchers are very excited at the prospect of interrogating that data.
But Epic's approach – anonymizing files containing the most sensitive information imaginable, about millions of people, and then releasing them to third parties – is a nightmare. "De-identified" data-sets are notoriously vulnerable to "re-identification" and the threat of re-identification only increases every time there's another release or breach, which can used to reveal the identities of people in anonymized records. For example, if you have a database of all the prescribing at a given hospital – a numeric identifier representing the patient, and the time and date when they saw a doctor and got a scrip. At any time in the future, a big location-data breach – say, from Uber or a transit system – can show you which people went back and forth to the hospital at the times that line up with those doctor's appointments, unmasking the person who got abortion meds, cancer meds, psychiatric meds or other sensitive prescriptions.
The fact that anonymized data can – will! – be re-identified doesn't mean we have to give up on the prospect of gleaning insight from medical records. In the UK, the eminent doctor Ben Goldacre and colleagues built an incredible effective, privacy-preserving "trusted research environment" (TRE) to operate on millions of NHS records across a decentralized system of hospitals and trusts without ever moving the data off their own servers:
https://pluralistic.net/2024/03/08/the-fire-of-orodruin/#are-we-the-baddies
The TRE is an open source, transparent server that accepts complex research questions in the form of database queries. These queries are posted to a public server for peer-review and revision, and when they're ready, the TRE sends them to each of the databases where the records are held. Those databases transmit responses to the TRE, which then publishes them. This has been unimaginably successful: the prototype of the TRE launched during the lockdown generated sixty papers in Nature in a matter of months.
Monopolies are inefficient, and Epic's outmoded and dangerous approach to research, along with the roadblocks it puts in the way of clinical excellence, epitomizes the problems with monopoly. America's health care industry is a dumpster fire from top to bottom – from Medicare Advantage to hospital cartels – and allowing Epic to dominate the EHR market has somehow, incredibly, made that system even worse.
Naturally, Kuttner finishes out his article with some antitrust analysis, sketching out how the Sherman Act could be brought to bear on Epic. Something has to be done. Epic's software is one of the many reasons that MDs are leaving the medical profession in droves.
Epic epitomizes the long-standing class war between doctors who want to take care of their patients and hospital executives who want to make a buck off of those patients.

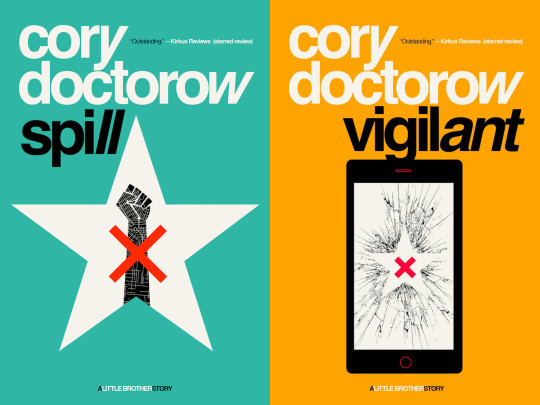
Tor Books as just published two new, free LITTLE BROTHER stories: VIGILANT, about creepy surveillance in distance education; and SPILL, about oil pipelines and indigenous landback.

If you'd like an essay-formatted version of this post to read or share, here's a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2024/10/02/upcoded-to-death/#thanks-obama

Image: Flying Logos (modified) https://commons.wikimedia.org/wiki/File:Over_$1,000,000_dollars_in_USD_$100_bill_stacks.png
CC BY-SA 4.0 https://creativecommons.org/licenses/by-sa/4.0/deed.en
#pluralistic#ehrs#robert kuttner#tres#trusted research environments#ben goldacre#epic#epic systems#interoperability#privacy#reidentification#deidentification#thanks obama#upcoding#Hierarchical Condition Category#medicare#medicaid#ai#American Recovery and Reinvestment Act#HITECH act#medicare advantage#ambient listening#alert fatigue#monopoly#antitrust
819 notes
·
View notes
Text

The Global Cardiac Biomarkers Market size was valued at USD 8.42 billion in 2019 and is predicted to reach USD 28.29 billion by 2030, with a CAGR of 11.6% from 2020-2030.
#Cardiac Biomarkers#Cardiac Biomarkers Market#Cardiac Biomarkers Industry#Myocardial muscle Creatine Kinase#Troponins (T and I)#Myoglobin#Brain Natriuretic Peptide (BNPs) or NT-proBNP#Ischemia Modified Albumin (IMA)#Myocardial Infarction#Congestive Heart Failure#Acute Coronary Syndrome#Atherosclerosis#Point of care testing#Laboratory testing
0 notes
Text
https://www.worldwisepeople.net/main/blogs/334425/Heart-Failure-Drugs-Market-Trends-Strategic-Assessment-Research-Size-Share
Heart Failure Drugs Market Top Players, Demands, Overview, Component, Industry Revenue and Forecast 2030
#Heart Failure Drugs Market Top Players#Demands#Overview#Component#Industry Revenue and Forecast 2030
0 notes
Text
https://facekindle.com/read-blog/163689
Heart Failure Drugs Market Opportunities, Growth Potential, Demand, Future Estimations and Statistics 2030
0 notes
Text
Blood Test Could Identify Heart Failure Relapse Risk
According to a study from Johns Hopkins University in the United States, a routine blood test could predict the likelihood of congestive Heart Failure Pipeline Market in patients who have a high risk of relapse and readmission after hospital discharge. According to a study from Johns Hopkins University in the United States, routine blood tests could predict the likelihood of congestive heart failure in patients who have a high risk of relapse and readmission after hospital discharge. The study looked at 241 heart failure patients.
Between June 2006 and April 2007, 241 patients with heart failure who were admitted to Johns Hopkins Hospital were analyzed by researchers.
The levels of the protein known as N-terminal pro-B-type natriuretic peptide (NT-proBNP), which is thought to be a marker for heart stress, were measured in the patients upon admission and upon discharge.
For additional bits of knowledge on the Heart Failure Pipeline Market, Download a FREE example
Levels of NT-proBNP have been linked to an increase in adverse outcomes and a correlation with symptoms of heart failure in previous studies.
Patients whose protein levels dropped by less than 50% during their hospital stay were 57% more likely to be readmitted or die within a year, according to the study. Patients whose protein levels dropped by a greater percentage were also found to have higher mortality rates.
They went on to say that testing for NT-proBNP at the beginning and end of a patient's stay could help determine which patients are ready to leave and which ones are more likely to relapse and return to the hospital.
0 notes
Link
0 notes
Text
https://tannda.net/read-blog/76385_congestive-heart-failure-drugs-market-size-overview-share-and-forecast-2031.html
The Congestive Heart Failure Drugs Market in 2023 is US$ 7.21 billion, and is expected to reach US$ 12.98 billion by 2031 at a CAGR of 7.60%.
#Congestive Heart Failure Drugs Market#Congestive Heart Failure Drugs Market Overview#Congestive Heart Failure Drugs Market Scope
0 notes